Adult day service centers (also called “adult day care”) provide social stimulation for adults who need supervision due to a physical disability, frailty, or dementia, and a much-needed break for family caregivers.
Adult day service centers (also called “adult day care”) provide social stimulation for adults who need supervision due to a physical disability, frailty, or dementia, and a much-needed break for family caregivers.
My mother, Judy, had vascular dementia and Alzheimer’s disease. When she moved in with me and my young family in 2005, she could still do a lot by herself, but when I left every morning to go to work she was bored and depressed. She was also not eating. I didn’t realize until much later that Mom could not remember to look for the meals I left for her in the refrigerator, and that she could not follow my instructions to heat them in the microwave. I hired a neighbor to visit with Mom (and encourage her to eat), but that was only a few hours a week. Mom also refused to accept the invitations of other neighbors to go out for lunch or to activities such as concerts. Feeling self-conscious about her memory loss, she was isolating herself. How could I help her feel more engaged and less lonely? And how could I stop worrying about her all day long while I was at work?
At my local Office for the Aging I heard about an adult day service center at a nearby assisted living facility. Like most adult day service centers, this program provided activities such as discussion groups, reading out loud, exercise, music, and art, along with meals and snacks. Unfortunately, when I showed Mom the brochure she refused to go. If she had not moved into assisted living shortly after our conversation, I’m sure I would have suggested the program again.
Common questions about adult day service centers:
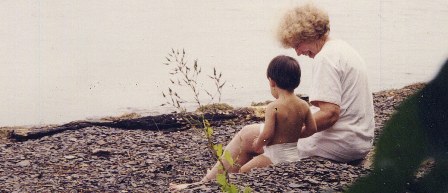
 Story time with visiting children, at Millennium Day Care in ArkansasAre these programs only for people with dementia? No, adult day service centers are open to any adult who needs supervision or assistance because of a physical disability, frailty, or cognitive impairment. Some programs, however, are more oriented toward people with Alzheimer’s disease and other dementias.
Story time with visiting children, at Millennium Day Care in ArkansasAre these programs only for people with dementia? No, adult day service centers are open to any adult who needs supervision or assistance because of a physical disability, frailty, or cognitive impairment. Some programs, however, are more oriented toward people with Alzheimer’s disease and other dementias.
What is the cost, and how can I pay for it?
Average daily fees run from $40 to $60. About 30% of adult day center participants pay privately. People attending these programs are eligible for funding from a number of sources including Medicaid-waiver programs, Veteran's contracts, and several federal entitlement programs. Guidelines for receiving these funds vary by state. Adult day service centers are usually covered by private long-term care insurance once that insurance is triggered by the person needing help with at least two “activities of daily living” (dressing, bathing, toileting, etc.) or needing supervision for their safety because of a cognitive impairment. Your local Office for the Aging should be able to help you figure out what funds are available.
Read more (posted on caregivers.com)
 Tuesday, October 1, 2013 at 07:40PM
Tuesday, October 1, 2013 at 07:40PM  "Caregiver Support" by The Animated WomanI love this drawing by “The Animated Woman” (called “Caregiver Support,” and shared here with permission). The person in the middle is both caring for the person on the left and being supported by the person on the right. As caregivers we need this kind of support, don’t we? It’s like a chain—the beginning of what is sometimes called a “circle of care.”
"Caregiver Support" by The Animated WomanI love this drawing by “The Animated Woman” (called “Caregiver Support,” and shared here with permission). The person in the middle is both caring for the person on the left and being supported by the person on the right. As caregivers we need this kind of support, don’t we? It’s like a chain—the beginning of what is sometimes called a “circle of care.”