Book Review: "Leaving Tinkertown"
 Monday, December 9, 2013 at 06:14PM
Monday, December 9, 2013 at 06:14PM  I just finished a memoir that I highly recommend for anyone who has a loved one living with Alzheimer's disease or another dementia. Beautifully written, and devastating in its detail, “Leaving Tinkertown,” by Tanya Ward Goodman, is both a first-rate father-daughter love story and a testament to the particular heartbreak that is early-onset Alzheimer’s disease.
I just finished a memoir that I highly recommend for anyone who has a loved one living with Alzheimer's disease or another dementia. Beautifully written, and devastating in its detail, “Leaving Tinkertown,” by Tanya Ward Goodman, is both a first-rate father-daughter love story and a testament to the particular heartbreak that is early-onset Alzheimer’s disease.
Although Tanya describes her father as disappearing before her eyes--and I usually don't recommend books that depict people with dementia as "gone" and no longer themselves--I think that this memoir reflects a truth of early-onset Alzheimer's disease: that it can be much more devastating in its brutality and swiftness than, perhaps, late-onset Alzheimer's.
Tanya's father, Ross, is an eccentric but gentle and nurturing man who made his living in the West as a painter for carnivals. Over the years Ross built a 22-room museum of miniature wooden scenes and figurines—Tinkertown—by adding rooms one by one to their farmhouse in New Mexico, building the walls from glass bottles and cement. Tanya grows up sharing her home with visitors from across the country. When her father is diagnosed at age 58 with Alzheimer’s disease, Tanya is barely scraping by in her late 20s in Los Angeles, but doesn’t hesitate to come home, leaving her sweetheart behind, to help out her father, who grows increasingly testy and stubborn, and her high-octane but emotionally-removed step-mother.
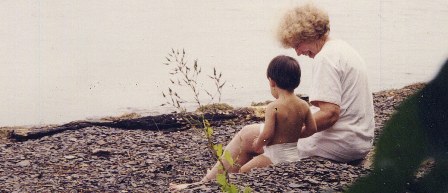
 The author of "Leaving Tinkertown," Tanya Ward Goodman, with her father, Ross
The author of "Leaving Tinkertown," Tanya Ward Goodman, with her father, Ross
In “Leaving Tinkertown” Tanya artfully weaves scenes from her childhood with those from the present, showing us how she continues to adore her father but struggles with the fears we so often have as caregivers—that she’ll forget who she is and what she wants for herself, or be overcome by sadness. She is angry that with his dementia her father “is leaving,” and angry that she is “being left.” Over time, Tanya learns not only how to find her place as an adult in this strange and unpredictable household, overcoming attacks of anxiety and self doubt, but how to find her strength as a daughter and caregiver.
As a reader, I came to feel a great fondness for both her and her father, so it was difficult to witness his rapid descent into early-onset Alzheimer’s. As the daughter of a woman who suffered from dementia for over 10 years, but declined more slowly than Ross and passed away at 80, not in middle-age, I felt immense sorrow for Tanya that she lost her father so young. Fortunately, her story is beautifully wrought; with exquisite detail, honesty and humor, Tanya guides us gently from moment to moment, in much the same way she learns to guide her father through the movements of his day. I highly recommend this book for any reader, not just those who have a loved one with dementia. Ross, Tanya, and the special place that is Tinkertown will stay with you long after you finish the last page.